Information re diet and supplements claimed to assist brain function: it is not unreasonable to optimise nutrition with regular fish, and seeds (especially flax "linseed") and walnuts to maximise omega 3 intake. A high dose multi vitamin and mineral supplement from the pharmacy could also be considered, but should not be too expensive. This supplement might include Omega 3, Vitamin B5 (pantothenic acid) >100mg, choline (or phosphatidyl choline) >500mg, phosphatidyl serine >30mg, pyroglutamate >250mg, DMAE (dimethylaminoethanol) >100mg daily. It is important to note that such supplementation is not supported by high quality trials. Low vitamin D levels are associated with weaker performance in cognitive tests in published research, the reason behind this is unclear.
Nutrition and supplements to assist sleep if that were a contributing problem. Calcium (600mg), Magnesium (400mg) pyridoxine (Vitamin B6, 100mg) and zinc (10mg) might help. If a tranquillising agent is needed she could trial Tryptophan (5-HTP, 1-200mg). Again, the scientific evidence is weak, and costs should be minimised.
All brain toxins should be avoided. This certainly includes alcohol (although 1 standard unit per day is healthier than none), and other recreational drugs. Many medications could affect cognition, but in particular Amitriptyline, Dothiepin, Nortiptyline and other tricyclic agent often used for sleep or pain can increase the risk and the symptoms fo dementia. Sedatives (benzodiazepine sleeping tablets, or Zopiclone, opiates eg codeine, tramadol, morphine) and Gabapentin amongst others can affect memory. Alcohol is likely the worst offender, although the effects of other recreational products can also harm the brain. Statins for cholesterol are now recognised to sometimes cause brain power loss and this is reversible if removed.
A high level of academic achievement appears protective. A positive effect of physical exercise has been demonstrated on those suffering memory loss. Brain teaser puzzles which continually change, and even exercise on uneven surfaces to keep the brain alert may be helpful.
Those at high risk of dementia generally include those at risk of heart attack and stroke. It might be inferred that even minor "strokes" (silent events seen only on MRI scans) are too much of a burden for some patients brains to compensate for. In particular, it has been proven that there is an association between dementa incidence and …
Current smokers were 70% more likely than those who had never smoked to develop dementia.
blood pressure were 60% more likely (esp younger ~55yrs old)
diabetes were more than twice as likely
raised fasting Homocysteine levels (ideal <9.2; the population median)
apolipoprotein E genetic status
cholesterol levels, even modestly high
Aspirin and other NSAIDs appear protective (potentially through anti-inflammatory mechanisms but also potentially through preventing stroke events). However, Aspirin for healthy adults in general does more harm than good unless specifically indicated.
On the basis of "stroke prevention = dementia prevention" other lifestyle issues that protect against stroke should also be considered. They are described below…
aim for a blood pressure <120/80 through lifestyle modification.
oThis will involve regaining high level of aerobic fitness with three hours per week puffing and sweating exercise, gradually built up to over a period of weeks to months.
oA low salt diet: aim to remove salt from the table and from the kitchen and remove salt from supermarket products purchased, aiming for <200 mg of sodium per serving and generally favouring low salt products although a small volume high salt products are not unreasonable.
oMedications such as ACEinhibitors are unlikely to be required at this level.
fresh fruit and vegetable intake, raw as much as possible, at least 6-9 servings per day.
Fish 3 servings per week, and optimise omega 3 intake instead by capsules (EPA equivalent of 1200mg) purchased from the chemist, or by flaxseeds (linseed) from the supermarket
avoid saturated fats particularly animal fats though should not be shy of vegetable fats such as nuts, seeds, soy, avocado or other vegetable products (but cannot fry food as the oils become toxic).
body mass index excellent range = 22.5 to 25, waist circumference satisfactory if < 93 centimetres (men) and 88cm (women)
For high cholesterol (LDL) statins like lipex and lipitor are proven to protect against stroke. One may wish to supplement with a low dose of Co-enzyme Q10 to protect muscles against toxicity of the statins. If the HDL (bad cholesterol) and TG (fats) are disturbed Niacin (Vit B3)may be required (begin low, build slow). (up to 40% reductions, but lesser 10% effect on LDL) There is robust evidence that these blood markers are important in vascular disease. They can be improved, and there is some evidence that this is effective in reducing vascular events, including when added to Statins. Nicotinic acid (Mega-dose Niacin or Vitamin B3, but not Nicotinamide not Inositol) is a cheap older (4 decades) drug to achieve this, which can be built up very slowly from 50 or 100mg tablet daily towards 500-1500mg twice daily (or same total doses three times daily). It usually causes an itchy red flushing 20+ minutes after the dose which can be intense. This effect is aborted by 25 to 300mg aspirin a half hour before the dose, but the flushing wears off when the body adjusts over time. The most concerning potential side-effect is Liver failure (but this mainly occurs with "no flush" long-acting forms of niacin). Therefore regular blood tests are required in the first 1 year, beginning at or before 6 weeks into treatment. Other side-effects, particularly at high doses are icthyosis (dry itchy skin), other skin rash, low platelets, impaired glucose tolerance, and impotence (although some claim it as beneficial for this). It is claimed to assist sleep and lower blood pressure, but there is no good evidence to support this. Another medication called Acipimox is also subsidised, is a derivative of Niacin and is similarly effective but does not appear to impact on blood sugar control (ie better for diabetes). Foods which MAY help raise HDL include Cranbury juice, soluble fibre (eg porridge or Metamucil), red wine, fish, oatbran, onions, soy products, apples, grapes, citrus,eggs. The evidence for this benefit is limited.
Other supplements such as high dose Vitamin C, Magnesium (300mg equivalent), Lysine, and a Multivitamin and mineral product are unproven for vascular protection but may have some uses. I do not recommend them on a scientific basis.
Homocysteine: is a powerful marker of risk for arterial disease (similar to smoking), tends to get worse with age (generally thought to represent worse nutrition). It is also associated with increased rates of dementia across the population. The studies show that Homocysteine-lowering is not an appropriate treatment for ischaemic heart disease (MI or angina patients possibly suffering worse symptoms), but is effective for stroke prevention. The main factors to reduce Homocysteine are B-vitamins. Supplements with Folate 2000 mcg daily (1/2 a 5mg tablet is close enough, and can be prescribed or "over the counter" at the chemist), B12 drops or "spots" 50-500 mcg under the tongue (Clinician's brand of supplements make a dropper bottle of liquid form, 50mcg/drop, Twinlabs make a pastille 'spot" 500mcg) and pyridoxine 25-50mg daily (this is easily available in B-vitamin supplements but can also be prescribed) can powerfully lower the Homocysteine, and are not expensive, purchased at the chemist. These substances can also be obtained from the diet, but generally at lesser amounts than can be supplemented. A diet high in Folate (fruit, uncooked vegetables and wholegrain cereals), B12 (animal products, avoid proton pump inhibitors if possible) and Pyridoxine (Brewer's yeast, Wheat bran, Wheatgerm, Oats, Mackerel, Sardines, Beef, Poultry, Avocado, Bananas, Brown rice, Dried fruits, Cabbage, Molasses, eggs) may provide homocysteine reductions and additional protective effects over and above the taking of vitamin pills effect on Homocysteine alone. Less well validated treatments to lower such a high homocysteine could include Tri-methyl glycine (TMG) 3-6 grams per day and zinc 20mg/day.
Examining patterns of dietary intake is illuminating. It may be that such patterns are effective because of direct brain protection, but it may be they are simply associated with a large range of other healthy life-choices which make the difference (eg not smoking, exercising, and maintaining a healthy weight). A study such as this is important, but cannot answer all the questions we might have.
Dietary Pattern Associated With Reduced Alzheimer's Disease Risk published online April 12 in the Archives of Neurology. The study will also appear in the June issue of the journal. April 23, 2010 — Individuals who consume a diet rich in nuts, fish, poultry, vegetables, fruits, and olive oil–based salad dressings but low in high-fat dairy products, red meat, organ meats, and butter have a reduced risk for Alzheimer's disease, a new study suggests. The finding, from a prospective community-based cohort study, warrants further exploration of food combinations in the prevention of this important public health problem, said lead study author Yian Gu, PhD, from the Taub Institute for Research in Alzheimer's Disease and the Aging Brain, Columbia University, New York City. "Many studies have looked at the relationship between diet and the risk of Alzheimer's disease, but they have tended to focus on single nutrients or dietary items, such as fruits or vegetables or intake of meats. But the reality is that people eat a variety of foods, so we wanted to determine the best combination that might prevent Alzheimer's," she told Medscape Neurology.
Nutrition and supplements to assist sleep if that were a contributing problem. Calcium (600mg), Magnesium (400mg) pyridoxine (Vitamin B6, 100mg) and zinc (10mg) might help. If a tranquillising agent is needed she could trial Tryptophan (5-HTP, 1-200mg). Again, the scientific evidence is weak, and costs should be minimised.
All brain toxins should be avoided. This certainly includes alcohol (although 1 standard unit per day is healthier than none), and other recreational drugs. Many medications could affect cognition, but in particular Amitriptyline, Dothiepin, Nortiptyline and other tricyclic agent often used for sleep or pain can increase the risk and the symptoms fo dementia. Sedatives (benzodiazepine sleeping tablets, or Zopiclone, opiates eg codeine, tramadol, morphine) and Gabapentin amongst others can affect memory. Alcohol is likely the worst offender, although the effects of other recreational products can also harm the brain. Statins for cholesterol are now recognised to sometimes cause brain power loss and this is reversible if removed.
A high level of academic achievement appears protective. A positive effect of physical exercise has been demonstrated on those suffering memory loss. Brain teaser puzzles which continually change, and even exercise on uneven surfaces to keep the brain alert may be helpful.
Those at high risk of dementia generally include those at risk of heart attack and stroke. It might be inferred that even minor "strokes" (silent events seen only on MRI scans) are too much of a burden for some patients brains to compensate for. In particular, it has been proven that there is an association between dementa incidence and …
Current smokers were 70% more likely than those who had never smoked to develop dementia.
blood pressure were 60% more likely (esp younger ~55yrs old)
diabetes were more than twice as likely
raised fasting Homocysteine levels (ideal <9.2; the population median)
apolipoprotein E genetic status
cholesterol levels, even modestly high
Aspirin and other NSAIDs appear protective (potentially through anti-inflammatory mechanisms but also potentially through preventing stroke events). However, Aspirin for healthy adults in general does more harm than good unless specifically indicated.
On the basis of "stroke prevention = dementia prevention" other lifestyle issues that protect against stroke should also be considered. They are described below…
aim for a blood pressure <120/80 through lifestyle modification.
oThis will involve regaining high level of aerobic fitness with three hours per week puffing and sweating exercise, gradually built up to over a period of weeks to months.
oA low salt diet: aim to remove salt from the table and from the kitchen and remove salt from supermarket products purchased, aiming for <200 mg of sodium per serving and generally favouring low salt products although a small volume high salt products are not unreasonable.
oMedications such as ACEinhibitors are unlikely to be required at this level.
fresh fruit and vegetable intake, raw as much as possible, at least 6-9 servings per day.
Fish 3 servings per week, and optimise omega 3 intake instead by capsules (EPA equivalent of 1200mg) purchased from the chemist, or by flaxseeds (linseed) from the supermarket
avoid saturated fats particularly animal fats though should not be shy of vegetable fats such as nuts, seeds, soy, avocado or other vegetable products (but cannot fry food as the oils become toxic).
body mass index excellent range = 22.5 to 25, waist circumference satisfactory if < 93 centimetres (men) and 88cm (women)
For high cholesterol (LDL) statins like lipex and lipitor are proven to protect against stroke. One may wish to supplement with a low dose of Co-enzyme Q10 to protect muscles against toxicity of the statins. If the HDL (bad cholesterol) and TG (fats) are disturbed Niacin (Vit B3)may be required (begin low, build slow). (up to 40% reductions, but lesser 10% effect on LDL) There is robust evidence that these blood markers are important in vascular disease. They can be improved, and there is some evidence that this is effective in reducing vascular events, including when added to Statins. Nicotinic acid (Mega-dose Niacin or Vitamin B3, but not Nicotinamide not Inositol) is a cheap older (4 decades) drug to achieve this, which can be built up very slowly from 50 or 100mg tablet daily towards 500-1500mg twice daily (or same total doses three times daily). It usually causes an itchy red flushing 20+ minutes after the dose which can be intense. This effect is aborted by 25 to 300mg aspirin a half hour before the dose, but the flushing wears off when the body adjusts over time. The most concerning potential side-effect is Liver failure (but this mainly occurs with "no flush" long-acting forms of niacin). Therefore regular blood tests are required in the first 1 year, beginning at or before 6 weeks into treatment. Other side-effects, particularly at high doses are icthyosis (dry itchy skin), other skin rash, low platelets, impaired glucose tolerance, and impotence (although some claim it as beneficial for this). It is claimed to assist sleep and lower blood pressure, but there is no good evidence to support this. Another medication called Acipimox is also subsidised, is a derivative of Niacin and is similarly effective but does not appear to impact on blood sugar control (ie better for diabetes). Foods which MAY help raise HDL include Cranbury juice, soluble fibre (eg porridge or Metamucil), red wine, fish, oatbran, onions, soy products, apples, grapes, citrus,eggs. The evidence for this benefit is limited.
Other supplements such as high dose Vitamin C, Magnesium (300mg equivalent), Lysine, and a Multivitamin and mineral product are unproven for vascular protection but may have some uses. I do not recommend them on a scientific basis.
Homocysteine: is a powerful marker of risk for arterial disease (similar to smoking), tends to get worse with age (generally thought to represent worse nutrition). It is also associated with increased rates of dementia across the population. The studies show that Homocysteine-lowering is not an appropriate treatment for ischaemic heart disease (MI or angina patients possibly suffering worse symptoms), but is effective for stroke prevention. The main factors to reduce Homocysteine are B-vitamins. Supplements with Folate 2000 mcg daily (1/2 a 5mg tablet is close enough, and can be prescribed or "over the counter" at the chemist), B12 drops or "spots" 50-500 mcg under the tongue (Clinician's brand of supplements make a dropper bottle of liquid form, 50mcg/drop, Twinlabs make a pastille 'spot" 500mcg) and pyridoxine 25-50mg daily (this is easily available in B-vitamin supplements but can also be prescribed) can powerfully lower the Homocysteine, and are not expensive, purchased at the chemist. These substances can also be obtained from the diet, but generally at lesser amounts than can be supplemented. A diet high in Folate (fruit, uncooked vegetables and wholegrain cereals), B12 (animal products, avoid proton pump inhibitors if possible) and Pyridoxine (Brewer's yeast, Wheat bran, Wheatgerm, Oats, Mackerel, Sardines, Beef, Poultry, Avocado, Bananas, Brown rice, Dried fruits, Cabbage, Molasses, eggs) may provide homocysteine reductions and additional protective effects over and above the taking of vitamin pills effect on Homocysteine alone. Less well validated treatments to lower such a high homocysteine could include Tri-methyl glycine (TMG) 3-6 grams per day and zinc 20mg/day.
Examining patterns of dietary intake is illuminating. It may be that such patterns are effective because of direct brain protection, but it may be they are simply associated with a large range of other healthy life-choices which make the difference (eg not smoking, exercising, and maintaining a healthy weight). A study such as this is important, but cannot answer all the questions we might have.
Dietary Pattern Associated With Reduced Alzheimer's Disease Risk published online April 12 in the Archives of Neurology. The study will also appear in the June issue of the journal. April 23, 2010 — Individuals who consume a diet rich in nuts, fish, poultry, vegetables, fruits, and olive oil–based salad dressings but low in high-fat dairy products, red meat, organ meats, and butter have a reduced risk for Alzheimer's disease, a new study suggests. The finding, from a prospective community-based cohort study, warrants further exploration of food combinations in the prevention of this important public health problem, said lead study author Yian Gu, PhD, from the Taub Institute for Research in Alzheimer's Disease and the Aging Brain, Columbia University, New York City. "Many studies have looked at the relationship between diet and the risk of Alzheimer's disease, but they have tended to focus on single nutrients or dietary items, such as fruits or vegetables or intake of meats. But the reality is that people eat a variety of foods, so we wanted to determine the best combination that might prevent Alzheimer's," she told Medscape Neurology.
Dr. Gu and her colleagues studied a cohort of 2148 elderly subjects 65 years and older living in New York City. All subjects were healthy and free of dementia at study entry. Their dietary habits were obtained via questionnaire, and they were prospectively evaluated with the same standardized neurologic and neuropsychological measures approximately every 1.5 years for an average of 4 years.
The researchers used reduced rank regression to calculate dietary patterns according to their effect on 7 nutrients previously shown in the literature to be related to Alzheimer's disease: saturated fatty acids, monounsaturated fatty acids, omega-3 polyunsaturated fatty acids, omega-6 polyunsaturated fatty acids, vitamin E, vitamin B 12, and folate.
During the follow-up, 253 individuals developed Alzheimer's disease. The study found that one dietary pattern — characterized by higher intakes of salad dressing, nuts, fish, tomatoes, poultry, cruciferous vegetables, fruits, and dark and green leafy vegetables and a lower intake of high-fat dairy products, red meat, organ meat, and butter — was significantly associated with a reduced risk for Alzheimer's disease.
Compared with subjects in the lowest tertile of adherence to this pattern, the Alzheimer's disease hazard ratio (95% confidence interval) for subjects in the highest tertile was 0.62 (0.43 – 0.89) after multivariable adjustment ( P = .01).
The study also found that subjects who were older, less educated, and current smokers tended to be less adherent to the protective diet. Hispanic individuals adhered less than white and black individuals ( P = .02), and women tended to adhere more than men (P = .05)."The dietary pattern that was most protective against Alzheimer's reflected a diet rich in ω-3 and ω-6 polyunsaturated fatty acids, vitamin E, and folate but poor in saturated fatty acids and vitamin B12," commented Dr. Gu. "The combination of nutrients in this dietary pattern reflects multiple pathways in the development of Alzheimer's disease. "For example, vitamin B12 and folate are homocysteine-related vitamins that may have an impact on the disease through their ability to lower circulating homocysteine levels," she said. "Vitamin E is a strong antioxidant, and the fatty acids may be linked to dementia and cognitive function through atherosclerosis, thrombosis, or inflammation. Fatty acids may also affect brain development and membrane functioning." She added that the study has several limitations. "We used a single measurement of the diet, and this might not have captured the long-term dietary habits of the subjects. We also excluded subjects from the final analysis because they were lost to follow-up, and this might have introduced selection bias. We also can't completely rule out the possibility that the reduced risk associated with this protective diet was due to residual confounding." Further studies are planned, Dr. Gu said. "We cannot say based on this study alone that this type of dietary pattern prevents Alzheimer's disease, but many studies have consistently shown that fruits and vegetables and unsaturated fatty acids are associated with a lower risk. We want to repeat these findings in different populations and see if they can be confirmed in other studies."
Array of Health Behaviors ; Commenting on this study for Medscape Neurology, David Knopman, MD, professor of neurology at the Mayo Clinic and a member of the Mayo Clinic Alzheimer's Disease Research Center in Rochester, Minnesota, said that, despite the study authors' best efforts, it is still not clear whether diet alone makes a difference. "Dietary habits, which often are lifelong, are certainly part of the array of health behaviors that contribute to better cognitive health in late life. However, diet and other health behaviors are intertwined. Because a healthy diet contributes to better cardiac health, lower weight, lower blood pressure and a lower risk for diabetes, there are many reasons to view the dietary habits described by Dr. Gu and colleagues as beneficial."
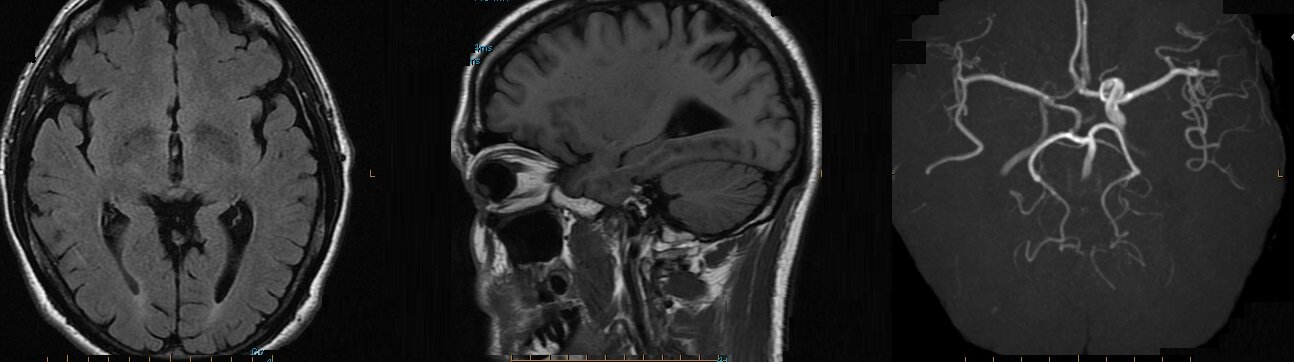
Fish consumption improved brain volume in the frontal lobes, temporal lobes (including the hippocampus) and posterior cingulate gyrus, as shown on high-resolution, three-dimensional volumetric magnetic resonance imaging (MRI). "That's important because these are areas of the brain that are responsible for memory and learning and are severely affected by Alzheimer's disease," reported Dr. Cyrus A. Raji of the University of Pittsburgh. Dr. Raji and his colleagues analyzed data collected at three time points from the ongoing Cardiovascular Health Study-Cognition Study. In 1989-1990, 260 subjects (mean age 71 years) completed standardized diet questionnaires. In 1998-1999, these individuals (mean age 78 years) underwent volumetric MRI. An analysis of clinical conversion to mild cognitive impairment (MCI) or Alzheimer's disease (AD) in 2002 among study participants (mean age 82 years) found that individuals with larger brain volumes as a result of weekly baked or broiled fish consumption had a greatly reduced incidence of MCI or AD, compared with individuals who did not eat fish regularly. Clinical conversion rates to MCI or AD were 30.8% for non–fish eaters, compared with 8% for individuals whose brains benefited partially from fish consumption (as shown on volumetric MRI), and 3.2% for individuals whose brains benefited fully from fish consumption. These findings indicate "a large reduction in the risk for developing AD or MCI as a result of consuming baked or broiled fish," Dr. Raji said The benefits of regular fish intake persisted even after accounting for such potential confounding variables as age, gender, head size, and cerebrovascular disease. Study participants who were not fish eaters and who showed atrophy in the hippocampus – the region most frequently affected by AD – had a 47% incidence of MCI or AD, compared with only 28% of fish eaters with larger hippocampal volumes, he reported. In addition, mean scores on cognitive tests of working memory were significantly higher (P less than .05) in individuals who ate fish weekly compared with those who did not. The improvement remained even after accounting for potential confounders such as age, gender, and education. The researchers also looked at cognitive test scores and brain volumes and found a relationship between larger frontal lobe volumes in fish eaters and higher working memory test scores. "This makes a lot of sense, because the frontal lobes are responsible for working memory function," Dr. Raji said. The reduced risk of MCI and AD among fish eaters in this study probably stems from the protective benefits of omega-3 fatty acids, he noted. Omega-3 fatty acids are believed to increase blood flow to the brain, act as antioxidants and anti-inflammatories, and prevent the accumulation of the amyloid plaques characteristic of AD. Consumption of fried fish, which is high in cholesterol and low in omega-3 fatty acids, did not confer any benefits.Data presented by Dr. Raji at last year's meeting of the Radiological Society of North America (Internal Medicine News, Dec. 20, 2010) showed the protective benefits of physical activity in preserving brain volume and reducing the risk of AD and MCI in the same cohort. "What we're adding to the picture this year is specific information on diet," he said. "The long-term goal of this research is to incorporate our understanding of all the various lifestyle factors that could reduce risk and give us a unified picture of how to best prevent the disease." Dr. Raji had no disclosures related to this study.
From the emedicine website: A novel lifestyle intervention may reverse cognitive decline in AD patients. In a study of 10 patients with memory loss associated with either AD, mild cognitive impairment, or subjective cognitive impairment, researchers found that a personalized comprehensive lifestyle intervention tailored to address metabolic deficits identified on laboratory testing as affecting the plasticity of the patient's brain improved memory loss. Cognition subjectively or objectively improved in 9 of the 10 patients within 3 to 6 months. Although interventions were tailored to each patient, they all included elimination of simple carbohydrates from the diet, increased consumption of fruit, vegetables, and non-farmed fish, and adherence to a strict meal pattern with timed periods of fasting. All interventions also included an exercise program, counseling on stress reduction techniques, and use of a variety of daily supplements, including vitamin D3, fish oil, coenzyme Q10, melatonin, and methylcobalamin. Female patients were advised to resume previously discontinued hormone replacement therapy when appropriate.
Routine physical activity and exercise may have an impact on AD progression and may perhaps have a protective effect on brain health. Increased cardiorespiratory fitness levels are associated with higher hippocampal volumes in patients with mild AD, suggesting that cardiorespiratory fitness may modify AD-related brain atrophy. The activity of each patient should be individualized. The patient's surroundings should be safe and familiar. Too much activity can cause agitation, but too little can cause the patient to withdraw and perhaps become depressed. Maintaining structured routines may be helpful to decrease patient stress in regard to meals, medication, and other therapeutic activities aimed at maintaining cognitive functioning. The patient needs contact with the outside environment. The physician should encourage participation in activities that interest the patient and result in cognitive stimulation but do not stress the patient. The range of possibilities is wide and may include visits to museums, parks, or restaurants.
There are no proven modalities for preventing AD. Evidence, largely epidemiologic, suggests that healthy lifestyles can reduce the risk of AD. Physical activity, exercise, and cardiorespiratory fitness may be protective. A French study of 8,085 nondemented participants aged 65 years and older found that frequent consumption of fruits and vegetables, fish, and omega-3 rich oils may decrease the risk of dementia and AD, especially in APOE E4 noncarriers. Although no definitive dietary recommendations can be made, in general, nutritional patterns that appear beneficial for AD prevention fit the Mediterranean Diet. Following this type of diet, along with recommendations for physical activity, has the added benefit of lowering the risk of cardiovascular and metabolic disorders. Animal studies suggest that diets low in calories benefit cognitive function in old age. A German study of 50 healthy, normal-weight to overweight elderly patients found that 3 months of calorie restriction (30% reduction) resulted in a significant increase in verbal memory scores, which was correlated with decreases in fasting plasma levels of insulin and high sensitive C-reactive protein. The effect of calorie reduction on memory was most pronounced in patients with best adherence to the diet. Light to moderate alcohol consumption has been linked to reduced risk of development of AD. In contrast, a Finnish study found that abstainers, heavy drinkers, and binge drinkers had an increased risk of cognitive impairment when compared to light to moderate drinkers. Among abstainers, however, increased risk was limited to subjects who did not carry the APOE E4 allele.
The researchers used reduced rank regression to calculate dietary patterns according to their effect on 7 nutrients previously shown in the literature to be related to Alzheimer's disease: saturated fatty acids, monounsaturated fatty acids, omega-3 polyunsaturated fatty acids, omega-6 polyunsaturated fatty acids, vitamin E, vitamin B 12, and folate.
During the follow-up, 253 individuals developed Alzheimer's disease. The study found that one dietary pattern — characterized by higher intakes of salad dressing, nuts, fish, tomatoes, poultry, cruciferous vegetables, fruits, and dark and green leafy vegetables and a lower intake of high-fat dairy products, red meat, organ meat, and butter — was significantly associated with a reduced risk for Alzheimer's disease.
Compared with subjects in the lowest tertile of adherence to this pattern, the Alzheimer's disease hazard ratio (95% confidence interval) for subjects in the highest tertile was 0.62 (0.43 – 0.89) after multivariable adjustment ( P = .01).
The study also found that subjects who were older, less educated, and current smokers tended to be less adherent to the protective diet. Hispanic individuals adhered less than white and black individuals ( P = .02), and women tended to adhere more than men (P = .05)."The dietary pattern that was most protective against Alzheimer's reflected a diet rich in ω-3 and ω-6 polyunsaturated fatty acids, vitamin E, and folate but poor in saturated fatty acids and vitamin B12," commented Dr. Gu. "The combination of nutrients in this dietary pattern reflects multiple pathways in the development of Alzheimer's disease. "For example, vitamin B12 and folate are homocysteine-related vitamins that may have an impact on the disease through their ability to lower circulating homocysteine levels," she said. "Vitamin E is a strong antioxidant, and the fatty acids may be linked to dementia and cognitive function through atherosclerosis, thrombosis, or inflammation. Fatty acids may also affect brain development and membrane functioning." She added that the study has several limitations. "We used a single measurement of the diet, and this might not have captured the long-term dietary habits of the subjects. We also excluded subjects from the final analysis because they were lost to follow-up, and this might have introduced selection bias. We also can't completely rule out the possibility that the reduced risk associated with this protective diet was due to residual confounding." Further studies are planned, Dr. Gu said. "We cannot say based on this study alone that this type of dietary pattern prevents Alzheimer's disease, but many studies have consistently shown that fruits and vegetables and unsaturated fatty acids are associated with a lower risk. We want to repeat these findings in different populations and see if they can be confirmed in other studies."
Array of Health Behaviors ; Commenting on this study for Medscape Neurology, David Knopman, MD, professor of neurology at the Mayo Clinic and a member of the Mayo Clinic Alzheimer's Disease Research Center in Rochester, Minnesota, said that, despite the study authors' best efforts, it is still not clear whether diet alone makes a difference. "Dietary habits, which often are lifelong, are certainly part of the array of health behaviors that contribute to better cognitive health in late life. However, diet and other health behaviors are intertwined. Because a healthy diet contributes to better cardiac health, lower weight, lower blood pressure and a lower risk for diabetes, there are many reasons to view the dietary habits described by Dr. Gu and colleagues as beneficial."
Regular fish intake lowers dementia risk
December 2, 2011, BY SUSAN BIRK CHICAGO (EGMN) – Consumption of baked or broiled fish on a weekly basis improved brain health and significantly reduced the risk of mild cognitive impairment and Alzheimer's disease in a 20-year longitudinal study of older adults presented at the annual meeting of the Radiological Society of North America.Fish consumption improved brain volume in the frontal lobes, temporal lobes (including the hippocampus) and posterior cingulate gyrus, as shown on high-resolution, three-dimensional volumetric magnetic resonance imaging (MRI). "That's important because these are areas of the brain that are responsible for memory and learning and are severely affected by Alzheimer's disease," reported Dr. Cyrus A. Raji of the University of Pittsburgh. Dr. Raji and his colleagues analyzed data collected at three time points from the ongoing Cardiovascular Health Study-Cognition Study. In 1989-1990, 260 subjects (mean age 71 years) completed standardized diet questionnaires. In 1998-1999, these individuals (mean age 78 years) underwent volumetric MRI. An analysis of clinical conversion to mild cognitive impairment (MCI) or Alzheimer's disease (AD) in 2002 among study participants (mean age 82 years) found that individuals with larger brain volumes as a result of weekly baked or broiled fish consumption had a greatly reduced incidence of MCI or AD, compared with individuals who did not eat fish regularly. Clinical conversion rates to MCI or AD were 30.8% for non–fish eaters, compared with 8% for individuals whose brains benefited partially from fish consumption (as shown on volumetric MRI), and 3.2% for individuals whose brains benefited fully from fish consumption. These findings indicate "a large reduction in the risk for developing AD or MCI as a result of consuming baked or broiled fish," Dr. Raji said The benefits of regular fish intake persisted even after accounting for such potential confounding variables as age, gender, head size, and cerebrovascular disease. Study participants who were not fish eaters and who showed atrophy in the hippocampus – the region most frequently affected by AD – had a 47% incidence of MCI or AD, compared with only 28% of fish eaters with larger hippocampal volumes, he reported. In addition, mean scores on cognitive tests of working memory were significantly higher (P less than .05) in individuals who ate fish weekly compared with those who did not. The improvement remained even after accounting for potential confounders such as age, gender, and education. The researchers also looked at cognitive test scores and brain volumes and found a relationship between larger frontal lobe volumes in fish eaters and higher working memory test scores. "This makes a lot of sense, because the frontal lobes are responsible for working memory function," Dr. Raji said. The reduced risk of MCI and AD among fish eaters in this study probably stems from the protective benefits of omega-3 fatty acids, he noted. Omega-3 fatty acids are believed to increase blood flow to the brain, act as antioxidants and anti-inflammatories, and prevent the accumulation of the amyloid plaques characteristic of AD. Consumption of fried fish, which is high in cholesterol and low in omega-3 fatty acids, did not confer any benefits.Data presented by Dr. Raji at last year's meeting of the Radiological Society of North America (Internal Medicine News, Dec. 20, 2010) showed the protective benefits of physical activity in preserving brain volume and reducing the risk of AD and MCI in the same cohort. "What we're adding to the picture this year is specific information on diet," he said. "The long-term goal of this research is to incorporate our understanding of all the various lifestyle factors that could reduce risk and give us a unified picture of how to best prevent the disease." Dr. Raji had no disclosures related to this study.
From the emedicine website: A novel lifestyle intervention may reverse cognitive decline in AD patients. In a study of 10 patients with memory loss associated with either AD, mild cognitive impairment, or subjective cognitive impairment, researchers found that a personalized comprehensive lifestyle intervention tailored to address metabolic deficits identified on laboratory testing as affecting the plasticity of the patient's brain improved memory loss. Cognition subjectively or objectively improved in 9 of the 10 patients within 3 to 6 months. Although interventions were tailored to each patient, they all included elimination of simple carbohydrates from the diet, increased consumption of fruit, vegetables, and non-farmed fish, and adherence to a strict meal pattern with timed periods of fasting. All interventions also included an exercise program, counseling on stress reduction techniques, and use of a variety of daily supplements, including vitamin D3, fish oil, coenzyme Q10, melatonin, and methylcobalamin. Female patients were advised to resume previously discontinued hormone replacement therapy when appropriate.
Routine physical activity and exercise may have an impact on AD progression and may perhaps have a protective effect on brain health. Increased cardiorespiratory fitness levels are associated with higher hippocampal volumes in patients with mild AD, suggesting that cardiorespiratory fitness may modify AD-related brain atrophy. The activity of each patient should be individualized. The patient's surroundings should be safe and familiar. Too much activity can cause agitation, but too little can cause the patient to withdraw and perhaps become depressed. Maintaining structured routines may be helpful to decrease patient stress in regard to meals, medication, and other therapeutic activities aimed at maintaining cognitive functioning. The patient needs contact with the outside environment. The physician should encourage participation in activities that interest the patient and result in cognitive stimulation but do not stress the patient. The range of possibilities is wide and may include visits to museums, parks, or restaurants.
There are no proven modalities for preventing AD. Evidence, largely epidemiologic, suggests that healthy lifestyles can reduce the risk of AD. Physical activity, exercise, and cardiorespiratory fitness may be protective. A French study of 8,085 nondemented participants aged 65 years and older found that frequent consumption of fruits and vegetables, fish, and omega-3 rich oils may decrease the risk of dementia and AD, especially in APOE E4 noncarriers. Although no definitive dietary recommendations can be made, in general, nutritional patterns that appear beneficial for AD prevention fit the Mediterranean Diet. Following this type of diet, along with recommendations for physical activity, has the added benefit of lowering the risk of cardiovascular and metabolic disorders. Animal studies suggest that diets low in calories benefit cognitive function in old age. A German study of 50 healthy, normal-weight to overweight elderly patients found that 3 months of calorie restriction (30% reduction) resulted in a significant increase in verbal memory scores, which was correlated with decreases in fasting plasma levels of insulin and high sensitive C-reactive protein. The effect of calorie reduction on memory was most pronounced in patients with best adherence to the diet. Light to moderate alcohol consumption has been linked to reduced risk of development of AD. In contrast, a Finnish study found that abstainers, heavy drinkers, and binge drinkers had an increased risk of cognitive impairment when compared to light to moderate drinkers. Among abstainers, however, increased risk was limited to subjects who did not carry the APOE E4 allele.